PaJR was birthed on the day humans started journaling their life.
PaJR was birthed on the day humans started journaling their life. All books, all biographies and all memoirs invariably are medical case reports or journals. Your autobiographical being, which sees you in 3rd person is your own perception of how you behave, how you emote and how you perceived things. Diseases are not simply diagnoses and a set of numbers which need to be treated, they are experiences, emotions and shape lives in every possible way, particularly in India, wherein the owner of the disease alone does not experience the disease, it is their family, friends or anyone invested in them who experiences the disease with them. A disease here in India is a diagnosis for a collective unit!
This forms or should form the very bedrock on which medical practice should be based. As with most systems, which initially start off clean, the stakeholders in the system eventually change and lead it to a different direction and thus pivot and respond to a completely unrelatable set of incentives. However, one thing has and will very likely remain constant in any healthcare system – that patients are the most important stakeholders, and they want their outcomes improved for which they seek healthcare. Therefore, patients’ outcomes have to be at the centre of all decision-making.
Most systems have in fact started off with the same goal and incentive, however as with any system and human life in itself – rust sets in and corruption ensues. Therefore, antifragility of the most important stakeholder is paramount.
To build antifragile systems, patients should ideally be their own doctors and be able to take completely rational, logical and evidence-based decisions for their own best outcomes. However, for a myriad of reasons this is not possible (many linked to political systems) and it is a well-known fact that doctors make some of the worst patients!
So how do we solve this? Within current operating models, we can begin by educating patients on disease patterns and how they are influencing outcomes in them. This is best explained by using Bloom’s taxonomy to understand levels of learning. Here is an image of Bloom’s taxonomy and let us conceptualise it to an individual patient –
To begin with, a medical consultation begins with the patient presenting a set of chief concerns to the doctor and the doctor subsequently asking the patient a set of questions based on these initial chief concerns. There are two possible roadblocks here – one, the patient having poor recall or poor understanding of the doctor’s questions and two, the doctor being “incompetent” in asking the right questions or allowing the consultation to evolve further
Assuming both roadblocks are navigated successfully, as the consultation progresses, patient demonstrates understanding of their disease, and this is easily assessed by their answers to the classic questions – “what makes it better and what makes it worse”, “at what time of the day are symptoms worse” etc.
“We had lunch in two parts: at 1:30 pm with a little rice, fenugreek greens, jute spinach and cabbage curry, and a little while ago, we had a shradh: two puris, chickpea dal, two slices of paneer, fried potatoes, fruit chutney, a rasgulla and some sweet curd. In the evening, we had to attend another Eid invitation. At 5:30 p.m., we boarded the auto and left for the place of invitation, about seven kilometres away, and reached about six o’clock. After a while, we enjoyed a bowl of Simai payas and a sweet. It was about nine o’clock when we returned home after eating dinner with meat and rice at eight o’clock.” – A 63 year old gentleman with breathlessness and hypertension since 2 years
As the doctor gains this information, they apply (quite often pattern recognition from subconsciously programmed system 1 reasoning – link it) critical thought and try to make the patient understand the problem. There could be several
potential pitfalls here – one, is the doctor trained enough on recognising the pattern closest to the truth, two – is the doctor only relying on system 1 (fast, illogical and reflexive) thinking or deliberately applying system 2 reasoning (slow, logical and rational), three – is the doctor able to communicate their thinking and reasoning to the patient and check their understanding, and four – the patient is also at step 3 with the doctor and already have their own understanding of the disease (and a diagnosis which either they are hoping or most scared of) – are the patient and doctor in agreement on their understanding of the patient’s disease.
Analysis is the step where doctors often have to apply system 2 reasoning and battle against their own system 1 reasoning trying to overpower their system 2! This is often the hardest step for most practitioners, and plenty tend to wither away here. The potential pitfalls here are endless!
Once the level of ‘analyse’ is breached, rational thinking takes over. The consultation is progressing as these are happening and the doctor now has the patient’s trust (assuming all roadblocks are navigated successfully) and is evaluating their next steps. The patient is conscious of the thought that the doctor has deliberated on the information given by me and that subsequent options suggested by them are now in my best interests.
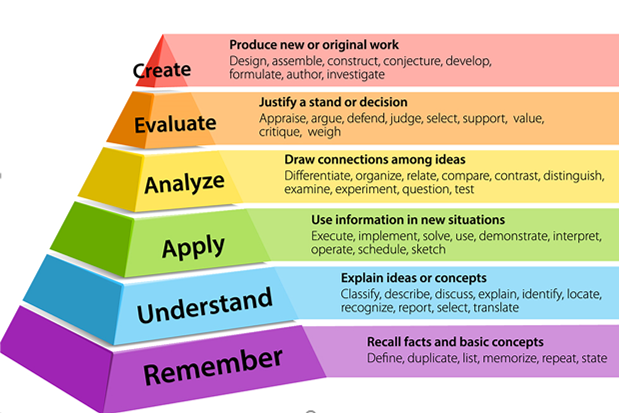
Sourced from – Pyramid-for-Blooms-Taxonomy.png (619×413)
Learning and knowledge can only be created – which is the ultimate level of learning – only longitudinally as things progress. Because creation of new information and data, in the context of a medical consultation needs follow-up to evaluate the first consultation. Patients report their outcomes, create their own entirely unique and highly individual narrative with their illness. The doctor eventually chooses to report this narrative in the form of case reports or as part of larger studies.
This, my dear reader is the heart and soul of PaJR! This is what placing patients at the heart of healthcare means and this is how I believe doctors should practice, this is how students should be trained, and this is how individuals patients are empowered, made accountable and autonomous and eventually spontaneously are involved in shaping societies and politics.
Core Team
Mrs. Sailaja G – Leading patient volunteer and advocate. Star member for taking the project forward
Ms. Lajrupa Bhadra – Leading patient volunteer and advocate.
Dr. Avinash Kumar – Doctor, writer, researcher, citizen science volunteer and innovator
Ms. Narmeen Shah – relentless pursuit in creating knowledge; committed and passionate about PaJR project
Dr. Vivek Poddar – Doctor, researcher and writer. Inspiration for medical students across continents
Dr. Himaja – Keen student and PaJR volunteer. Active researcher and future star.
Dr. Venkanna – Passionate about medical science, star PaJR volunteer
Dr. Praneeth Vatti – Doctor, innovator and dabbles with biomedical sciences. Active stakeholder in PaJR project.
Mr. Rahul Kulkarni – He is a seasoned product innovator and mentor having built teams and products across large organizations and startups. He is committed to developing patient centred PaJR ecosystems for global mentoring and local caring.
Above all – our patients who teach and inspire us to commit to our ideas, daily
SWOT (Strengths, weakness, opportunities, and threats) Analysis
by my professor and pioneer of PaJR
Strengths
Only cherry-picked information is shared. Only the success stories are presented. The success stories are our biggest strength for patient centred healthcare driven by patient outcomes.
He has written a book about this in the past. Here is the link to his book.
Here is the link to his other book on user-driven healthcare. This details how patients are the most important stakeholders in any healthcare system and their outcomes should be the primary drivers of all medical systems.
Weaknesses
A system is only as competent and efficient as it’s individual components and participants
Rhetoric: Practice, practice, practice! The only way to beat weakness toward strength and power is gaining regular knowledge through a life long journey of self-directed learning!
And self-learning and self-governance are at the very heart of what PaJR wants to achieve. We shall strive for it, all our lives!
Opportunities
Formal medical education has currently given up trying to encourage real patient centred interaction among medical students during their training phase such that for a few who may engage in it at some point in their careers (even after they become faculty) would realise that the very interaction with real patients who are also humans would be transformative in their understanding of humans (again not everyone may be able to do that on one’s own and there is an accepted dearth of faculty who can train people in doing that), which is the kind of training a real politician needs, to understand their polity and work for them rather than their own selves! It has been exemplified in the past by some well known political leaders! Read more on our conversation on why politics and medicine / healthcare are married to each other.
Here is our student winning an award for her exemplary case reporting on PaJR
Our group does this as a 24×7 regular journey through user driven healthcare (UDHC) tools such as PaJR and CBBLE (more about them in links below).
Threats
Thorns of clinical complexity amidst the guardrails
Picture taken from the garden after pruning the Indian jujube tree
Stakeholder trade-offs in negotiating virtual transparency accountability vs real threat to privacy and security!
Rhetoric: Healthcare is not easy! It’s a journey full of challenges and threats and yet a fantastic way to live life using science and technology to create one’s life work of art!
Links to the lecture preceding the demo: